Infertilty
Null tempus sollicitudin dui, ut vehicula lacus porta vel duis
urna ligula luctus at feugiat a lacinia ut sem.
Am I Infertile?
- Am I Infertile?
- Infertlity in Women
- Diagonosis for Women
- Infertility in Men
- Diagnosis for Men
- Am I Infertile?

Couples who fail to conceive after more than a year of unprotected sex (6 months for women over 35) are considered to have an infertility problem. While both men and women are at risk of some degree of infertility, women over the age of 35 are particularly at risk of fertility-related conditions.
Our practice specializes in treating and diagnosing these circumstances, and we invite all couples, especially at-risk couples, to check with our highly trained staff of fertility specialists to begin your family’s travel on the ideal foot.
The following are examples of symptoms that may affect a couple’s fertility, and if present, a consultation should be made before trying to conceive:

OriginElle Fertility Clinic & Women’s Health Centre:
the family dream becomes reality.
- Women with irregular or no menstruation
- Women with a history of pelvic infections, appendix surgeries or other thoracic/abdominal surgeries
- Women with severe pain during menstruation
- Couples with a history of miscarriages
- Couples with a history of sexually transmitted diseases
- Men who have had testicular surgery, injury, or childhood infections such as mumps
- Men with sexual issues such as premature ejaculation and/or erectile dysfunction
- Infertlity in Women

Infertility is the inability to conceive after one year of sexual intercourse without contraception, or after six months if the woman is over the age 35.
Infertility in men accounts for approximately 20% of fertility-related problems in a couple, while 50% of cases are due to infertility issues with the woman. In remaining cases, both the man and the woman are experiencing some measure of infertility.

Race has not proven to be a factor in infertility across the globe, though prevalence of STDs and later-age pregnancies have been showed to affect rates of infertility in the general population.
Abnormal bleeding
Abnormal menstrual bleeding relates to unusual menstrual bleeding before, during or after a woman’s menstrual period. Abnormal menses can be caused by hormone imbalance, or by more serious conditions such as uterine growths or uterine cancer.
Age related infertility
The age-related decline of a woman’s fertility is known as age related infertility. Beginning in her mid-20s and accelerating after she reaches her mid-30s, a woman’s fertility continuously declines, more so even after age 40. Middle-aged men are also less fertile than young men in their 20s.
Anovulation
When a woman’s ovaries do not develop and release eggs, this is known as anovulation. Accounting for approximately 25% of all infertility cases, anovulation is quite common. If a woman only has her period every few months, or none at all, she may not be ovulating or ovulating infrequently, thus causing infertility.
Cancer treatment
Cancer treatments including radiation and chemo therapy can have a major impact on fertility due to removal or damage to reproductive organs, eggs, and sperm. Prior to beginning cancer treatments or undergoing any surgery to your reproductive organs, both women and men should consult with our fertility specialists.
Ectopic pregnancy
An ectopic pregnancy occurs when a fertilized egg implants outside of the uterus, most times somewhere within the fallopian tube. This occurs when the fallopian tube is blocked or damaged. The fallopian tube of course cannot support the growing embryo, and the ectopic pregnancy may cause the tube to rupture and bleed, resulting in a potentially serious medical situation.
Endometriosis
Endometriosis is a condition where the tissue that lines the inside of the uterus (endometrium) is found outside the uterus. Endometriosis may grow on the outside of a woman’s uterus, ovaries, fallopian tubes, bladder or even intestines, interfering with the fertilization process or an embryo’s implantation thus causing infertility.
Exercise
Over exercising or lack of exercise are both linked to fertility problems in men and women.
Fibroids
Uterine fibroids are common and can affect embryo implantation and general fertility. Fibroids growing in the cavity of the womb (submucous) or distorting the lining of the womb (some intra mural) affect fertility. As many as 20% of women have fibroids during their childbearing years, and 50% of women will have fibroids by age 50..
Genetic causes of infertility in women
Many women are unable to conceive and deliver a healthy baby due to genetic factors as a result of inherited chromosome abnormalities or single-gene defects.
Hormone imbalance
The process of ovulation and implantation of a fertilized egg depends upon a complex balance of hormones and their interactions with each other. Any disruption in this process can hinder ovulation or the implantation of the fertilized egg in the uterine lining.
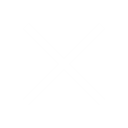
Male infertility
In approximately 40% of infertile couples, male infertility is either the sole cause or a contributing cause of infertility. Problems with the sperm’s shape, numbers, health and movement can affect the ability to conceive. Infertility may also result when there is a blockage or obstruction in the man’s vas deferens (small tubes that connect the testes to the man’s urethra), blocking sperm from exiting the body.
Miscarriage & repeated pregnancy loss
Repeated pregnancy loss is defined as 3 confirmed lost pregnancies prior to 20 weeks. Although approximately 25% of all pregnancies result in miscarriages, fewer than 5% of women will experience two consecutive miscarriages, and only about 2% experience three or more miscarriages. Tests are normally done after 2 miscarriages to determine if any medical causes are responsible for the repeated miscarriages.
Obesity
Obesity is a major risk factor for infertility. Ovulation may be affected by obesity and many eating-related disorders can alter the normal balance of hormones and affect fertility.
Polycystic ovarian syndrome (PCOS)
PCOS is a common cause of infertility. Severe hormonal imbalances cause eggs to remain immature, shrink and turn into cysts in the ovaries. The eventual buildup of cysts worsen hormonal imbalances.
Polyps
There are two types of polyps that affect fertility: uterine polyps (which are also referred to as endometrial polyps) and cervical polyps. Uterine polyps are masses or lesions of the uterine wall (the endometrium). Cervical polyps are smooth, finger-shaped growths in the cervix, which is the passage between the vagina and uterus. Polyps can affect the fertilization or embryo growth process.
Sexually transmitted diseases
STDs, particularly Chlamydia, can damage a woman’s fallopian tubes and cause infertility. Men may also experience decreased fertility as a result of STDs.
Smoking and alcohol
Smoking and excessive alcohol consumption may effect fertility both in females and males.
Stress and infertility
Some studies indicate that mental stress may affect ovulation and sperm production, thus causing infertility.
Tubal disease
Fertilization occurs in the woman’s fallopian tubes where sperm meets egg. This fertilized egg travels down the tube into the uterus, where it develops into a baby. Any blockage of the tubes is called tubal disease and will prevent sperm and egg from joining, or may cause ectopic pregnancy. Tubal disease accounts for about 35% of all infertility problems.
Unexplained infertility
Unexplained infertility is the diagnosis if all fertility tests are normal and the cause of infertility cannot be defined. In practice it is said to occur if semen analysis is normal, the woman is ovulating and fallopian tubes are open. Couples with unexplained infertility have a very high success rate with fertility treatments like intrauterine insemination (IUI) or in vitro fertilization (IVF).
Uterine abnormalities & malformations
Uterine abnormalities include uterine fibroids, polyps, adhesions and scar tissue, which can interfere with egg fertilization or embryo development.
Uterine adhesions
Adhesions (also known as Asherman syndrome) are bands of scar tissue that form between or inside of abdominal organs. In very severe cases, adhesions may obstruct or distort the inside of the uterus to the point where a fertilized egg may not be brought to full term.
- Diagnosis for Women

Blood tests
Blood tests determine hormone levels at critical points in the monthly cycle. For the reproductive cycle to occur, hormonal balance and timing are essential.
Miscarriage/recurrent pregnancy loss diagnosis
Ovarian reserve
The number of viable eggs in a woman’s ovaries is assessed by measuring blood levels of follicle stimulating hormone (FSH) and oestradiol (E2), anti-mullerian hormone (AMH) and inhibin B levels. An ultrasound scan can also be performed to measure the number of tiny follicles (eggs structures) in each ovary.
Ovulation testing
Uterus and fallopian tubes testing
Structural problems are tested and diagnosed by several minor procedures done in the physician’s office:
- Ultrasound and transvaginal ultrasound: A procedure that involves the use of high-frequency sound waves reflected off body structures to create images of reproductive organs; ultrasound is one of the simplest and least invasive fertility diagnostic tests and can clearly assess some conditions that cause infertility, like ovarian cysts, or polycystic ovaries (PCO), where the ovary contains more than twelve small follicles in the ovary. PCO must be distinguished from polycystic ovarian syndrome (PCOS). PCO occurs in 20-30 percent of the general population and the patient may have no symptoms at all. PCOS is said to occur if the woman has two of the following three conditions: PCO, irregular or infrequent menstrual cycles indicating anovulation, and/or evidence of elevated androgen (male hormone) levels. PCOS is reported in 2-3 percent of Canadian women.
- Sonohysterogram: A transvaginal ultrasound procedure that also fills the uterus with a saline solution to detect endometrial polyps, fibroids, or other problems inside the uterus. It can also check if the fallopian tubes are open by seeing if the saline spills out from the ends of the tubes and collects at the back of the uterus.
- Hysterosalpingography: A dye solution is injected into the uterus to see the contours of the uterus and whether the tubes are open. It is similar to the sono-HSG but generally more uncomfortable because of reaction to the dye solution.
- Hysteroscopy: A surgical procedure in which a small scope (camera) is inserted into the uterus through the cervix to look at the inside of the uterus in order to diagnose polyps, fibroids or adhesions that may be causing infertility. During hysteroscopy, these issues can be surgically removed.
- Laparoscopy: A surgical procedure in which a small camera and small surgical instruments are inserted into the pelvic region through the abdomen via two to five small incisions. This procedure may evaluate and remove endometriosis, adhesions and other scarring, polyps and blockages of the tubes.
Thyroid tests
A blood test for thyroid stimulating hormone (TSH) and thyroid antibodies is generally done to determine if TSH could be a factor of infertility. Treatment for this issue may include administration of synthroid (thyroid hormone replacement), if needed.
An earlier evaluation may be appropriate for women older than 35 who cannot become pregnant after six months of trying.
Early testing may also be appropriate for women who have a history of any of the following:
- Irregular menstrual cycles
- Absent or missing periods, suggesting no ovulation
- Recurrent miscarriages
- Prior abdominal surgery
- Prior cancer treatments
- Suspected problems with the uterus or fallopian tubes
- Ruptured appendix or severe pelvic infection, suggesting blocked fallopian tubes
Minimally invasive procedures, such as laparoscopy or hysteroscopy that involve scopes and cameras inserted into the abdomen, carry the usual low risks of minimally invasive surgery, including:
- Bruising and tenderness in the abdomen
- Risk of infection at the incision sites
- Possibility of an internal organ being pierced by a surgical tool
- Infertility in Men

The absence of sperm in the semen, low sperm counts and/or sperm that cannot reach the egg once ejaculated during intercourse are all causes of male infertility. Physical blockages can occur in the deferens tubes, either from a prior vasectomy or a failed vasectomy reversal.
Testosterone imbalance and other hormone conditions, as well as genetic or chromosomal issues that affect sperm production, viability, or motility can cause male infertility.
Impotence from spinal cord injuries or psychological/emotional traumas can also cause male infertility.
Unfortunately, problems with sperm production, delivery, or genetic and chromosomal disorders don’t necessarily have external symptoms and therefore can only be diagnosed by semen analysis and other specialized tests.
Testing
Semen can be collected by masturbation, electrical stimulation or by urological procedures that extract sperm directly from the testes, after which the sperm can be analyzed.
Sperm retrieval procedures, done under local or light sedation anesthesia, include Microepididymal Sperm Aspiration (MESA), Percutaneous Epididymal Aspiration (PESA), Testicular Excisional Sperm Aspiration (TESA), and Testicular Excisional Sperm Extraction (TESE). These procedures can also be used to extract sperm for later use for fertility treatment like in vitro fertilization (IVF), if necessary.
Genetic or chromosomal abnormalities can be determined by a blood test.
Treatment options
If sufficient healthy sperm can be retrieved, Intrauterine Insemination (IUI) can be performed where sperm are injected directly into the woman vagina.
Another treatment option is in vitro fertilization (IVF), where healthy sperm are used to fertilize a woman’s egg outside the womb and the resulting embryo is then implanted into the woman’s uterus.
Vasectomies can sometimes be reversed through microsurgery. However, if the man has a low sperm counts or sperm with low motility (sperm movement), IVF with ICSI (intracytoplasmic sperm injection), where one healthy sperm is directly injected into the egg, may be the best treatment.
In the case of genetic or chromosomal abnormalities, we have the technology to screen out abnormal sperm and keep only the healthy.
- Diagnosis for Men

A male fertility evaluation may include a physical exam to check for problems in the testicles, such as the absence of one or both testes, decrease in sizes of testes, testis mass that would suggest testicular cancer, or an enlargement in the veins in the scrotum (varicocele), a common cause of low sperm production.
A comprehensive semen analysis will determine the volume of sperm, number of sperm, portion of sperm that are able to move properly (motility), and number of sperm with healthy shape and structure (morphology) in a semen sample. Additional tests on the semen may include a test for antibodies in the semen that may kill or undermine sperm function or a test to analyze the sperm DNA integrity. Blood tests may be done to measure hormonal levels in the blood, which may be affect sperm production.
Generally, if a couple has tried unsuccessfully for one year to get pregnant, then fertility testing is recommended for both partners to determine the cause of infertility. However, a man may choose to get tested for infertility earlier if there is a known fertility-impact issue, such as:
- Cancer treatments in the past
- A genetic disorder like cystic fibrosis or congenital bilateral absence of the vas deferens (CBAVD)
- Impotence
- Previous surgery on testes, penis, or genito-urinary tract.
- A history of mumps in adulthood
- Trauma to the testicles, suggesting a potential sperm problem
- Known history of infertility or recurrent miscarriage
Blood tests for hormone analysis and semen/sperm analysis are virtually free of risk.
As with all surgical procedures, the risks of MESA, PESA, micro-TESE and TESA are small but can include:
- Bruising and tenderness in the scrotum
- Discomfort or pain
- Risk of infection in the incision area